Synthetic riboswitches can regulate gene expression and reduce antibacterial drug resistance and may increase the lifetime of traditional antibiotics, claim Chinese scientists.
Antibiotic resistance is a serious healthcare issue with gene transfer and mutations believed to be the most plausible causes. Antibiotics, such as penicillin, ampicillin, amoxicillin and cephalosporin have found widespread applications leading to increased exposure and in turn increased resistance. In these systems, the main route of resistance is the expression of beta-lactamase.
Here, the antibiotic is rendered inactive via a hydrolysis pathway of the beta-lactam ring. The discovery of new antibiotics and resistance pathway inhibitors has so far failed to keep up with the surge in antibiotic resistance. Therefore, researchers have looked at antisense agents, such as RNA, PNA and DNAzymes that combat drug resistance by inhibiting target genes.
However, these systems suffer from poor gene expression and have unknown toxicity effects.
Now, WANG Shu and colleagues at Chinese Academy of Sciences, Beijing, have turned their attention to riboswitches that are capable of controlled gene expression and have demonstrated that a synthetic riboswitch containing a theophylline-specific aptamer sequence can regulate the expression of beta-lactamase through theophylline-aptamer interactions, sharply reducing the antibiotic resistance of the engineered bacteria.
A riboswitch is a portion of an mRNA molecule and contains two parts: an aptamer and an expression platform. The aptamer contains the region that is capable of binding to a ligand and the expression platform modifies the gene expression when the ligand binds to the aptamer.
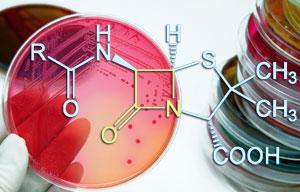
|
Drug resistance could be controlled using gene expression and not by finding new antibiotics (Image by ICCAS) |
'The novelty here is the construction of a synthetic riboswitch containing a theophylline-specific aptamer sequence for regulating the expression of beta-lactamase,' explains WANG. 'The non-antibiotic theophylline can be used as a co-agent to preserve the efficacy of traditional antibiotics and this new strategy may also provide as a useful tool for understanding antibiotic resistance-related bioprocess and gene regulation', he adds.
Tom Brown, an expert in bioorganic chemistry, at the University of Southampton, UK, comments, 'If the messenger-RNA for this enzyme could be destroyed, these bacteria would no longer be able to survive in the presence of beta-lactam antibiotics. This would have major consequences, as the efficacy of existing antibiotics against resistant bacterial strains would be restored.
But there are many stages to pass through before this approach can be considered for clinical use.
WANG says that the team now plans to focus the research on how to transfer engineered genes into pathogenic bacteria in order to control the antibiotic resistance of non-engineered pathogenic bacteria along with the construction of a synthetic riboswitch to control multi-drug resistance in bacteria or cancer cells. (RSC Publishing)





